Table of Contents
When a 27-year-old engineer walked into Dr Sandeep Vaishya's office with what seemed like an impossible diagnosis – 56 brain lesions – he would have been met with limited options and a grim prognosis a few years ago.
However, thanks to today’s advancements in radiation therapy technology and the astute guidance of the neurosurgeon from Fortis Hospital in Gurugram, the young man was treated and back home within days. This marked the first time in Asia that so many lesions were treated in a single session.
The Growing Cancer Burden in India
Cancer has become a ubiquitous health condition worldwide due to diverse causes. According to the National Centre for Disease Informatics and Research, India’s projected cancer burden is estimated to reach 29.8 million by 2025 [1]. And over the next decade, cancer incidence and mortality in the country are expected to increase, highlighting the need for enhanced prevention, early detection, and proper treatment strategies.
"An aging population, lifestyle changes, and increased longevity have resulted in a rise in cancer cases each year," notes Shankar Seshadri, Elekta India’s General Manager of Sales. Elekta develops precision radiation therapy devices and software and is at the forefront of cancer therapy. Cancer care management today has taken on a multimodal approach, with an estimated 60 percent of cancer patients requiring radiation therapy at some point in their treatment [2].
Evolution of Precision in Radiation Therapy
The fundamental challenge in radiation therapy has always been protecting healthy tissue while targeting cancerous cells.
This challenge drove decades of innovation, with Sweden's Elekta leading the charge in developing sophisticated radiation systems. Their breakthrough technologies turned what was once a blanket approach into a precise medical tool, capable of targeting tumours with remarkable accuracy while safeguarding surrounding healthy tissue.
Starting from basic X-rays in the 1890s [3], radiation therapy has progressed to sophisticated machines that can regulate targeted beams, with submillimetre precision, protecting healthy organs while treating tumours and controlling metastatic cancerous growth.
This journey from basic radiation to precision therapy marks one of medicine's most significant advances – turning a powerful but crude tool into an instrument of remarkable precision.
Advanced Radiation Therapy Technologies
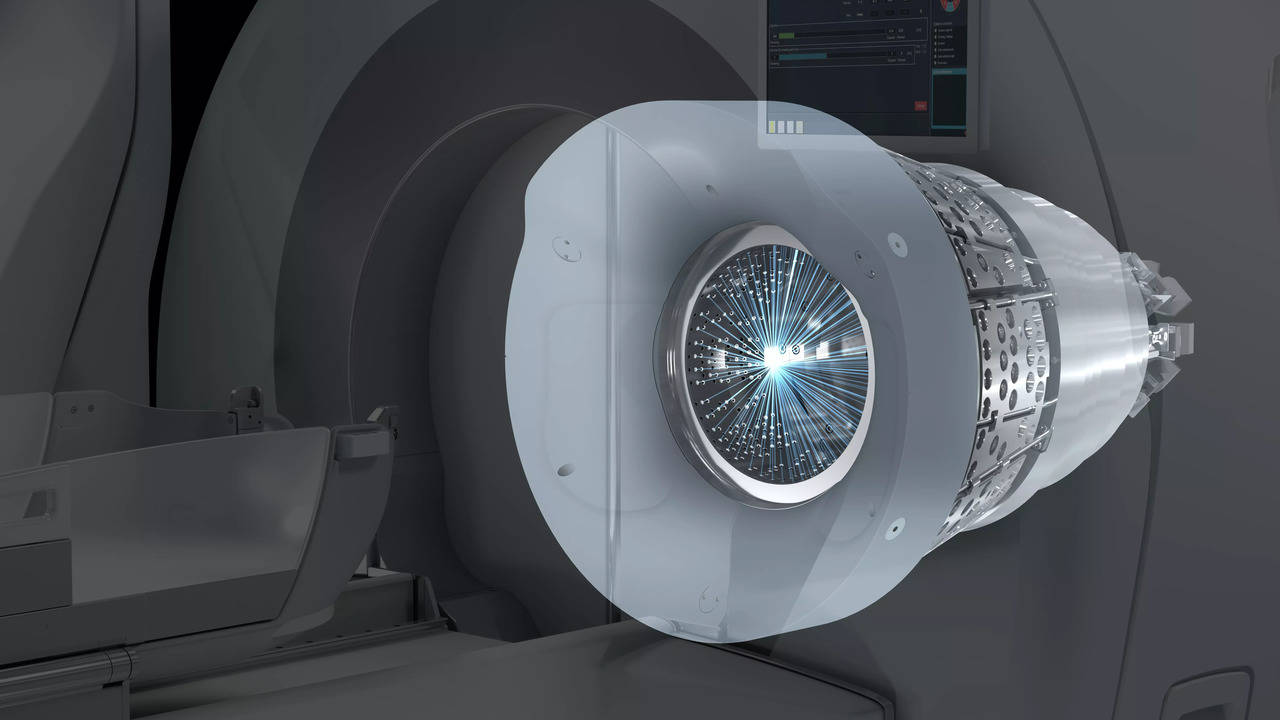
Radiation therapy has evolved to now include technologies such as linear accelerators (linacs), MR-Linac, and Gamma Knife, among others. Categorised as stereotactic radiation therapy or radiosurgery devices, these treat cancerous and noncancerous abnormalities in the body, without any incisions [4].
Stereotactic radiation therapy uses 3D imaging to target high doses of focussed radiation beams to the abnormal growth with minimal impact on the surrounding healthy tissue or organs. The high dose of radiation delivered to the affected area causes tumours to shrink and blood vessels to close off over time following treatment, robbing the tumour of its blood supply, and effectively removing it from the body.
Gamma Knife: Precision for Brain Treatment
Employing 192 small but precise gamma irradiation beams, Gamma Knife is not a knife, but a device with the precision of less than a tenth of a millimetre converging to a point. They deliver a radiation dosage while limiting the amount of radiation that reaches healthy tissue. Compared to standard brain surgery, this treatment’s non-invasive nature could result in a quicker recovery period. [5,10]. It was invented by Swedish neurosurgeon Lars Leksell and was taken forward by his son Larry Leksell as Elekta’s flagship product.
"Gamma Knife treats brain lesions, whether metastatic tumours, benign tumours, arteriovenous malformations, functional disorders like trigeminal neuralgia, obsessive-compulsive disorders, pain syndromes, and epilepsy," explains Dr Sandeep Vaishya, Fortis Hospital, Gurugram.
“If [a patient] can be treated with Gamma Knife, [they] can avoid major surgery and all the risk, complications, and the anxieties related to that. It is a pretty simple, safe, half-day procedure, [where the] patient comes in the morning, goes back home in the evening, [and] can lead a perfectly normal life,” adds Dr Vaishya.
Linac: Precision Treatment Almost Anywhere in the Body
Linear accelerators (linacs) are the most common device for precise radiation therapy for cancer. It works by accelerating electrons to deliver therapeutic X-rays to tumours. The linac machine moves around the patient, directing beams of radiation to specific points on the body. Using 3D image guidance with CT scans, linac systems are designed to target cancer cells while sparing surrounding tissue. Linac’s external beam radiation passes through the body, and hence doesn’t make the patient radioactive [13] .
Using a multileaf collimator (MLC) made of lead, it adapts to the shape of the treatment area. They can implement sophisticated techniques like intensity-modulated radiation therapy (IMRT) and volumetric modulated arc therapy (VMAT), delivering precise radiation exactly where needed [6].
MR-Linac: The Future of Radiation Therapy
MR-Linac combines magnetic resonance imaging (MRI) and linear accelerator radiation therapy, crucial for treating tumours in organs that move with breathing or digestion.
This device for real-time treatment allows the clinician to visualise the tumour or cancer in three-dimensional detail. The accuracy of the device allows the clinician to adjust the dose and radiation beams to the moving body to prevent any damage to surrounding tissue or organs. [9]
Compared to CT, MRI provides superior soft tissue contrast for both tumour and organs at risk (OARs) definition. A recent study showed MR-Linac treatment for lung cancer achieved 12-month local control rates of 95.6 percent, overall survival rates of 88 percent, and disease-free survival rates of 63.6 percent [7]. In the current scenario where lung cancer is the leading site for developing cancers in Indian males, the impact of MR-Linac is more relevant now than before [12]. Integrated MR-guided radiation therapy can reduce treatment sessions by up to 50 percent for some cancers while potentially improving outcomes [8].
Advancing Access to Care
This democratization of cutting-edge treatment means more patients can access world-class care within India. Institutions like Fortis Hospital Gurugram and Yashoda Hospital, Hyderabad now offer advanced MR-Linac technology. “But innovation alone isn’t enough,” stresses Elekta’s Senior Vice President Manikandan Bala, “We want to ensure that everyone has access to the advanced cancer care they deserve. That is our vision at Elekta.
While radiation therapy techniques continue to evolve, consultation with healthcare professionals remains essential for determining appropriate treatment options for individual cases.
(This is a partnered post)
References:
[1] National Centre for Disease Informatics and Research
[2] CancerCentre.com
[3] BBC – Bitesze (Advances in Medical Knowledge)
[4] Mayo Clinic – Stereotactic Surgery
[5] GammaKnife.com
[6] RadiologyInfo.org – Linear Accelerator
[7] Liu, X., Li, Z. & Yin, Y. Clinical application of MR-Linac in tumor radiotherapy: a systematic review. Radiat Oncol 18, 52 (2023). https://doi.org/10.1186/s13014-023-02221-8
[8] Kobika Sritharan, Alison Tree, MR-guided radiotherapy for prostate cancer: state of the art and future perspectives, British Journal of Radiology, Volume 95, Issue 1131, 1 March 2022, 20210800, https://doi.org/10.1259/bjr.20210800
[9] Hall WA, Paulson ES, van der Heide UA, et al. The transformation of radiation oncology using real-time magnetic resonance guidance: A review. Eur J Cancer. 2019. 11;(122):42-52.
[10] Gamma Knife® Surgery | Radiotherapy | Patients | Elekta
[11] MR-Linac & MRgRT Cancer Treatment | Patients | Elekta
[12] Sathishkumar, Krishnan et al. “Cancer incidence estimates for 2022 & projection for 2025: Result from National Cancer Registry Programme, India.” The Indian journal of medical research vol. 156,4&5 (2022): 598-607. doi:10.4103/ijmr.ijmr_1821_22
[13] Radiation Therapy Treatment | Patients | Elekta

